 |
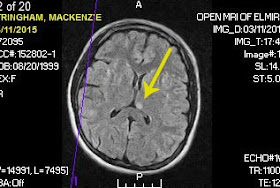
| The spot that started it all. |
I’m not myself. I haven’t been since
March 2015. That was when an imaging scan revealed a lesion on my then fifteen
year-old daughter’s brain. The scan was ordered to see why she was having increased headaches
and vision abnormalities associated with migraines. (During this past week’s
appointment at Golisano Children’s Hospital, I learned from the pediatric
neuro-oncologist that such findings are called an “incidental diagnosis.”) For
over a year, I have been walking a mental tightrope constructed of fear, sadness, and
anxiety. Although her pediatric neurologist, whom she’s been under the care of
for her epilepsy these past nine years, felt the lesion was going to turn out
to be “something boring,” he still referred her to a pediatric neurosurgeon at
a state and nationally ranked hospital for his official opinion. We left that
appointment with the same prognosis as her pediatric neurologist had given us; addressing
the brain anomaly as a lesion or scar tissue that she could have had since
development and that it appeared to pose no threat. Due to her autism and the
cognitive damage her grand mal seizure caused in 2014, the location of the
lesion, near her thalamus, hypothalamus, and brain stem, was deemed too
dangerous on both a cognitive and physiological level to risk a biopsy.
Six months later, we returned to the larger hospital for a comparison contrast MRI. Due to the mild reaction she had to contrast dye at our local facility, the MRI had to be performed at Golisano because they are better equipped for an adverse reaction. The contrast dye plays such a pivotal role in imaging lesions, her doctors agreed it was worth the risk to get the better images. She was prescribed Prednisone, an antihistamine, and Ativan ahead of the scan. We left the hospital for her across town follow-up appointment with the pediatric neurosurgeon. During the appointment, his vocabulary evolved since our initial appointment from lesion and scar tissue to glioma and tumor. My husband and I felt like we suffered a direct blow to our hearts. A medical sucker punch. We had been naïve. Maybe looking through rose-colored glasses during the first round of appointments. At any rate, I chastised myself for not jumping on the computer and researching as much as I could about brain lesions. If I had, I would have asked a lot more questions during the first visit. I realize doctors don’t want to make a patient and their family panic, especially when they feel the prognosis is positive, but I went into it blind and uninformed. I know how much doctors hate when patients or their family members use computers for self-diagnosis, however, being prepared isn’t a bad thing.
With the change in vocabulary, I researched
the terms and recommendations. My husband, while he was just as worried, wasn’t
freaking out like I was. He remained patient as I had my mom meltdowns fueled
by “what ifs?” I consulted with a friend who is an ER physician’s
assistant. In her department, she gets exposed to a little of everything. I
asked her if getting a second opinion was too extreme. She actually encouraged
it even if it was just for peace of mind. I arranged for a second opinion at Children’s Hospital of Philadelphia.
Their pediatric neurology and oncology departments are ranked third in the
nation. My daughter’s godmother’s mom let us spend the night at her house to
make the five hour trip to Philly a little easier on all of us. Staying with
her put us less than forty miles from the hospital. Their pediatric
neuro-oncologist agreed with our daughter’s doctors not only on the status of
the tumor, but reaffirmed that a biopsy would be detrimental to her. Mackenzie
isn’t the same child since her grand mal and we can’t risk losing more of her.
In March, Mackenzie traveled to
Rochester and had another six month comparison MRI. The neuro-radiologist and her
pediatric neurosurgeon concurred that her tumor appears to be stable and
unchanged. Upon getting her latest results, her pediatric neurosurgeon turned
Mackenzie’s future follow-ups and comparison imaging over to a pediatric
neuro-oncologist. Before meeting the new doctor, she had her routine six month
epilepsy check-up with her pediatric neurologist. During the visit, we
discussed her increased incidence of migraines with “Alice in Wonderland”
syndrome tendencies, her weight gain caused by her anti-seizure medication
(forty-eight pounds in two and a half years), and her memory issues (ßthank you, Grand Mal Seizure). On the
way home, I read over her computer printout from her visit notes. Under
"Problem List" it read: "Migraine with typical aura, Malignant
neoplasm of the brain, Generalized convulsive epilepsy, Congenital anomaly of
brain, Amnesia. “Malignant neoplasm of the brain?!” I was crushed. With
everything we’d been told, no one had used the M-word. Not once. We were told, “low
grade glioma of the thalamus, without midline crossing of the brain; clear edges
with no vascular involvement; size unchanged and stable.” I called the doctor’s
office en route to our home and asked the receptionist if a DX code had been
entered incorrectly since there had been no mention of a malignancy. She
assured me she would speak with the doctor since it needed to be fixed for
insurance purposes. My husband waited until the next day to call and make sure
it had been fixed. With everything going on, having an issue come up with our insurance
would be horrible. That was when she told him the doctor wanted to talk with us.
He called an hour later. It
boils down to there being too much “uncertainty" with her lesion and DX
code limitations. Since Kenzie is being referred to the pediatric neuro-oncologist
for further follow-ups and monitoring, her pediatric neurologist wanted to make
sure her paperwork was in order. The hospital’s computer doesn't allow for a
"middle of the road" diagnosis. A glioma is either benign or
malignant. There is no in between. While images showed no signs of growth
changes or indicated vascular involvement, the only 100% way to know would be
to biopsy and, as already stated, it isn’t an option.
This past week, we met with her
pediatric neuro-oncologist. He was a very nice man. Kenzie explained that she
was missing school because her teachers ended their strike the day before and
he went on to tell her how, when he was a student, he and his classmates went
on strike to protest the quality of the food served in their cafeteria. He
winked at her and told her that he was a student during the 60’s and protests
like that happened all the time. At any rate, he made us feel comfortable and
encouraged a lot of questions—from all of us. My college freshman daughter joined
us for the appointment. We’re a tight-knit family. What affects one of us,
affects all of us. While we chatted with the doctor, my thoughts focused on his
occupation. I couldn’t imagine having his job. While I know there have been
many breakthrough treatments, I still can’t imagine telling a family their child
has terminal cancer. Right now, Mackenzie isn’t part of that group. He seemed
very optimistic about her prognosis, but did acknowledge the difficulty “uncertainty”
caused for all concerned.
 |
| Do they come in a chocolate truffle flavor? |
This past year, even with some truly
great events occurring, has been shadowed by Mackenzie’s diagnosis. I try not
to dwell. God bless the creator of
Xanax! Without it, I’d never be able to focus coherently again, especially when
my mind goes around in what if circles. Uncertainty sucks. It rules your life.
Several times Mackenzie has asked me, “Why do all the bad things happen to me?” The kid has autism, epilepsy, migraines, and cognitive issues. And now she has a brain tumor. Seems like a fair question for her to ask. Only I don’t know how to answer her. Honestly, I barely have time to turn away from
her before she has a chance to see the tears welling in my eyes or the worry lines
appear on my face. I’ve become a hermit. I've isolated myself from others more than ever before—I’m
already an introvert. My poor husband takes the brunt of my turbulent emotions.
I usually snap at him and my patience level is pretty much non-existent. I have
great friends who keep telling me to remain optimistic and to focus on the
positive. I wish I knew how. I wish I knew how to turn some worry switch off inside
my brain to make such a feat possible. I lack this ability. Meanwhile, we go
forward and wait for the next six month comparison MRI.
As for productive writing, it doesn’t
come to me. I wanted to have my next book published in May. The book is only at the
halfway point. I simply can’t focus on writing. I hope my readers will continue
to be supportive and don’t forget about me.







